Introduction to the Scoring Matrix
You can’t score if you don’t know what your interviewers are assessing!
The Anaesthetics National Recruitment Office (ANRO) website publishes the interview scoring matrix. Despite the fact that there should be no mystery about what you are expected to demonstrate in the interview, many candidates find it difficult to distinguish a typical answer from an outstanding answer. This becomes clearer with practice and when you listen to how other candidates answer their questions. This article further fleshes out how to score well in each of the domains you are assessed in.
Firstly: Familiarise yourself with which domains are assessed in the Clinical Interview and which domains are assessed in the General Interview.
Table of Contents
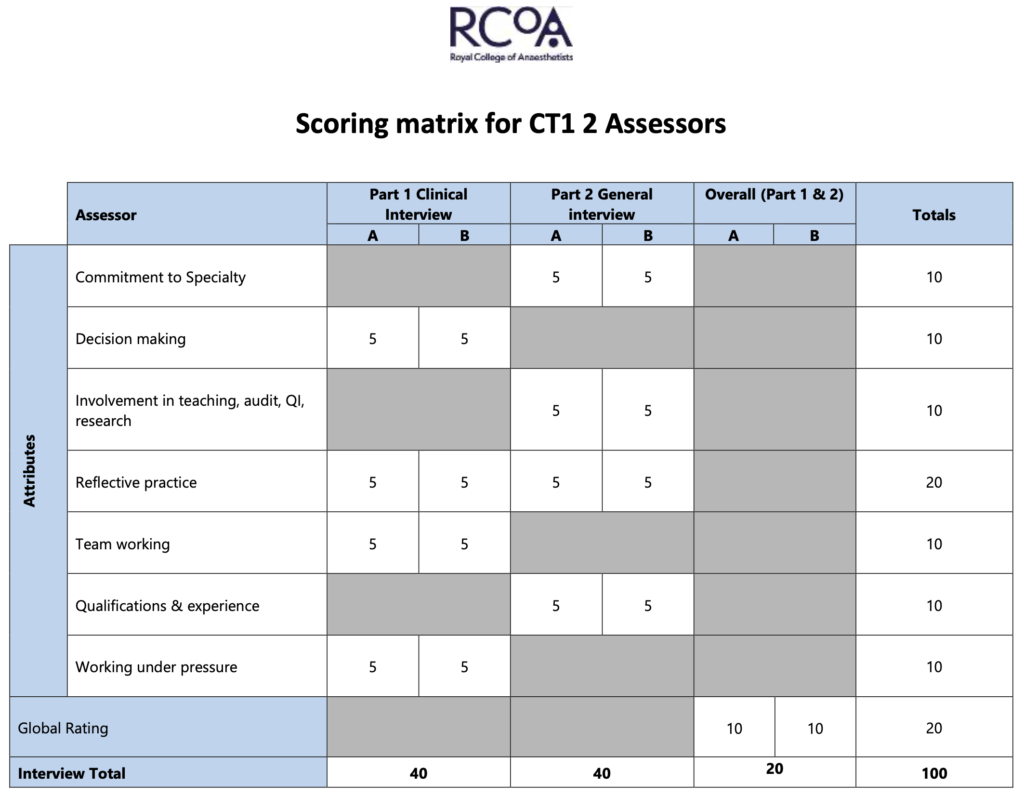
The domains being assessed in your Clinical interview are:
- Decision making
- Reflective practice
- Team working
- Working under pressure
The domains being assessed in your General interview are:
- Commitment to specialty
- Involvement in teaching, audit, QI, research
- Reflective practice
- Qualifications and experience
The rest of this guide will to through each domain in turn.
1. Clinical Judgement and Decision Making
Capacity to monitor developing situations, anticipate problems, and generate functional outcomes.
Descriptor: ‘Fully appreciated the wider needs of the situation & seeks team input’
- This should prompt candidates to demonstrate situational awareness when answering clinical questions. Simply saying that you would give an asthmatic patient ‘oxygen and nebulisers’ does not acknowledge the ‘wider needs’ of the situation
- An outstanding answer will also include an awareness of who else in the clinical team is able to help you execute the treatment plans and formulate differentials. It will also describe communication with the patient or any relevant carers.
- Be clear to explain which specific task you would ask which member of staff to carry out. Clearly it would be inappropriate to ask the porter to insert a cannula, but where roles and responsibilities can vary (eg. some nurses can carry out IV cannulation and others cannot), simply saying that you would ask each member what they are capable of doing will go a long way to demonstrate good team working on top of your decision making skills.
- Be mindful of where your scenario is set – if you are in an isolated location, mentioning that you need extra help or will have to call for help sooner will demonstrate good situational awareness.
Descriptor: ‘Was constantly alert to symptoms and signs which may destabilise patient’
- The age-old medical school mantra holds true here – if there is an obvious threatening abnormality, you should highlight it as soon as possible. For example, if your scenario includes a patient who has a GCS of 5/15, it is important that you mention a prompt airway assessment and an escalation for an airway-trained doctor to come to the scene.
- ‘Constantly alert’ implies that you should mention appropriate reassessments of the patient’s clinical circumstances to pick up on any deteriorations
Descriptor: ‘Regularly reviewed the situation and demonstrated forward planning’
- Simply saying that you will reassess a patient is only a typical answer. For an outstanding answer, you should mention what you are looking for in your reassessment and why. For example, in a case of acute asthma, you may consider saying that you would reassess their observations and ABG after commencing nebulizer therapy to find out if your treatment is working or if the patient is continuing to deteriorate in spite of it as escalation of care or planning for invasive ventilation may be necessary.
- ‘Forward planning’ does not only encompass escalation of clinical care to a senior or to another specialty. It also includes:
– where a patient should be treated (should you move them from majors to resus?),
– updating patients or carers (warning them that if they deteriorate they may require invasive ventilation so that when care is escalated it does not come as a big shock),
– and alerting theatres/ radiology/ cardiac catheterisation suite if a patient needs surgery/ scans/ stenting (these ‘special’ locations in the hospital require whole teams to be mobilised and forward planning means that you understand that these teams need to be set up and ready for your patient)
Descriptor: ‘Prioritised information and tasks. Personal plan of action. Appropriate help’
- In as much as is possible, structure your answers. Your interviewers will follow your answers more easily and thus award points for things you mention, and you will score more points for presenting yourself well under pressure as well as in the ‘global rating’.
- Part of structure is prioritising. Adopting an ABCDE approach in most cases will demonstrate good prioritisation. Be aware of other factors outside of the ABCDE structure that may be relevant in certain specific scenarios such as safeguarding, staff safety (aggressive patient), confidentiality – which may rank quite highly as a priority depending on the situation you are given.
- ‘Appropriate help’ is likely to be your registrar or consultant but do not forget other equally helpful team members: healthcare assistants, nurses, matrons, porters, physiotherapists, radiographers, specialist nurses and FY1 doctors.
Descriptor: ‘Took decisive and appropriate action to solve problems’
- In step with ‘prioritising information and tasks’, you are also expected to act on them accordingly (ie. treat the Airway before the Disability issue).
- Decisiveness is demonstrated in your prioritisation of your management steps. It is also communicated in your style of answer. Avoid saying ‘maybe’ or ‘might’ unnecessarily. Delegate tasks with assertiveness and clarity (for example, ‘I will ask the porter to deliver these blood samples to the laboratory for rapid group and screen and crossmatch while I continue assessing this patient’s bleeding’).
2. Reflective Practice
Reflective practice is much more than just ‘what went wrong – what I changed – what I do right now’. The reflective practice domain wants you to demonstrates how insightful you are into your own learning, weaknesses, strengths and ability to make plans to continue improving yourself (aka professional development). You should be able to talk about how certain events made you feel or how you think it may have made other team members feel.
This is the only domain to be assessed in both the Clinical and General Interviews, so you should pay close attention to developing reflective answers.
Educational Appraisal – how this has been used for professional development
Descriptor: ‘…evidence of regular educational review or appraisal with clear outcomes… concise examples of how these reviews have affected their personal development’
- Everyone will have had some form of an educational appraisal (think: educational or clinical supervisor meetings). You need to demonstrate insight into the importance of this process to your personal development to form an outstanding answer.
- Think of an example of when you spoke to a supervisor to come up with a plan on how you could improve your own skills/ knowledge/ practice. Explain how it has changed your practice for the better. You may find it useful to demonstrate that you made a SMART (specific, measurable, attainable, realistic, time-bound) goal to achieve this, if the interviewers ask for further details.
Risk Management – contribution to and understanding of risk management at a personal and NHS level
Descriptor: ‘… engagement in reducing risk in the workplace… insight into the impact of their own non-technical skills on the delivery of service and how they have taken measures to mitigate recognised issues’
- You will need to ‘describe and evidence’ your answers – DO NOT speak generally (eg. ‘audits are important’). Your answers should be about what YOU have done and should be specific to the questions (eg. ‘I enjoy participating in and heading Quality Improvement projects because… a project I have been involved in is…’)
- At an NHS level, risk management takes the form of checklists, M&M (morbidity and mortality) meetings and regular audits. You would also have had the opportunity to be involved in these at some level. You do not need to have been the person to uncover a massive systematic flaw in your trust to score well – you need only demonstrate direct involvement and awareness of where you fit in in the grand scheme of nationalised risk management strategies.
- You manage risk every day. As part of your preparation for your interview, try to be more conscious of the ‘little things that make a big difference’ that you have made part of your routine practice. Do you always call the lab to make sure they’re received an important group and screen sample? Do you have a method of making sure you’ve reviewed all your patient’s investigation results before discharging them? Do you make a shared jobs list at the start of each day so that the team work efficiently and safely?
- ‘Non-technical skills’ is a buzzword in anaesthesia and include communication, delegation, appropriate escalation… the list goes on! Think about a non-technical skill that is a particular strength and weakness of yours, and think of succinct examples you can talk about to evidence them if asked in your interview.
Personal Development Plans (PDPs) – appropriate use of PDPs… how they have influenced personal development
Descriptor: ‘…can account for the content of their Foundation PDPs. These should relate to the relevant foundation attachment… ideally demonstrate how their PDP enables career planning and shows commitment to specialty’
- This ties in closely with ‘Education Appraisal’. You need to demonstrate proactivity in creating relevant and useful PDPs. Employ SMART goals to bring structure to your answers.
- Most candidates are likely to talk about how they arranged a taster week in anaesthesia – you should go on to expand on how you arranged this, and what your goal was for that taster week (don’t just sound like you showed up for a week of shadowing, tell them what you wanted to learn from it and how you ensured you achieved it).
- You can and should also talk about PDPs ‘relevant to foundation attachment’. What did you try to learn from your cardiology/ renal/ surgical firms? All specialties interact with anaesthesia in some shape or form, so demonstrating a broad interest in other specialties and recognising that this will make you a better anaesthetist will form an outstanding answer.
Assessment Tools – maps assessment tools to evidence review and supports professional development
Descriptor: ‘can describe their use of workplace assessments (WPAs)… minimum of 2 assessment tools with evidence of how they have used them for practice and personal development’
- The table above already details the vast types of WPAs you can talk about in this section
- You must demonstrate some form of learning or development from these WPAs to gain an outstanding score. Simply mentioning that you do WPAs is insufficient. Have you ever done a case-based discussion on something tricky that you didn’t understand so that now you feel more confident approaching similar situations?
Feedback – demonstrates use of feedback
Descriptor: ‘more than one decisive example of feedback, which has resulted in a change in behaviour, advanced career development or improved clinical outcome’
- Start thinking of examples of when someone gave you constructive feedback and demonstrate your receptiveness to it and how it led to change.
- This does not necessarily need to be formal feedback in the form of an MSF. It could be as simple as a nursing colleague clarifying a hand-written prescription, which made you realise that your handwriting was not very clear so that now you are mindful of writing clearly in capital letters.
- You can also draw on feedback from senior colleagues or consultants, which has resulted in a change of practice.
- You should be sincere in your examples as the interviewers will be able to tell if you have just made up an example or did not genuinely learn from it!
3. Team Working
Capacity to work effectively with others and demonstrate appropriate leadership
Descriptor: ‘Ensured that capabilities of whole team matched tasks’
- Delegate appropriately
- Demonstrate awareness of subtle differences in confidence and abilities between staff of the ‘same role’ (eg. not all nurses are able to perform IV cannulation) by asking team members what they are confident and capable of doing.
Descriptor: ‘Always confirmed understanding & instructions, communicated plans clearly’
- In your answers, you should always mention checking the other person’s understanding
- ‘Closed-loop communication’ is where the team members confirm once a task has been done. You may choose to include this in your answers for your clinical interview
- Merely saying ‘I will communicate clearly’ does not demonstrate how you would do so. In your interview, you should give succinct examples of this. For example, ‘I will ask the ward nurse to bring me the resuscitation trolley with the defibrillator while I continue chest compressions on the patient’ is a much clearer than ‘I will ask the nurse to bring me the emergency equipment’.
Descriptor: ‘Remained very sympathetic & considerate to all other team members’
- This includes an awareness of when other teams are busy or under pressure when you are called to help
- If your clinical scenario includes anything that may be distressing, you may want to mention organising a hot or cold debrief and ensure that all participating team members receive the appropriate support
Descriptor: ‘Demonstrated leadership with authority & justification’
- Delegate appropriately (as discussed above)
- Explain to your team why you have made particular decisions and welcome discussions. Do not come across as the sort of person who will bulldoze their opinion the moment they are in the driver’s seat.
Descriptor: ‘Called for appropriate help with clear instructions’
- Firstly, you should know when to call for help. When in doubt, call for help – you are more likely to be penalised for not calling for help than you are for demonstrating some caution.
- Do not simply say ‘I will call for help’. You should be able to verbalise who or what help you need by saying, ‘I will pull the emergency buzzer and ask the nurse to put out a 2222 adult cardiac arrest call to our ward.’
Descriptor: ‘Maintained a very participative, non-confrontational approach’
- In your interview you should demonstrate that you are always open to listen to other team members’ opinions. You may even choose to say ‘I will ask if anyone else thinks I have missed anything’ as this will clearly demonstrate an open style of leadership.
- If, in your scenario, you are given a team member who is difficult to work with, you may find the SPIES mnemonic useful: Seek information, Patient safety, Initiative, Escalate, Support.
4. Working Under Pressure
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Ut elit tellus, luctus nec ullamcorper mattis, pulvinar dapibus leo.
Part of this domain assessment is what you say in your interview. The other part is how you come across in your interview. Be sure to speak at an appropriate pace, structure your answers and pause before starting your next answer. General nerves from the interview are acceptable – but if these nerves appear to affect your overall interview performance, you may see your score in this domain drop.
Capacity to make decisions under pressure and retain control. Awareness of own limitations.
Descriptor: ‘Seemed very relaxed & comfortable with demands of situation’
- Be aware that the ‘demands of the situation’ may be clinical as well as interactional.
- Approach any turns in your clinical interview as you would in real life. Ask for help when you normally would, and assess a patient as you normally would. Do not try anything heroic just because the context has shifted to an interview rather than real-life practice.
Descriptor: ‘Responded quickly & decisively to unexpected circumstances’
- This does not mean you need to answer the interviewers questions as though you are on The Chase! Pause after any question is asked, then deliver a succinct and decisive answer without any waffling.
Descriptor: ‘Maintained perspective throughout’
- This is fairly situation specific. What you will likely need to ‘maintain perspective’ about something in each scenario you are given. This could be potential safeguarding issues, logistical planning, staff safety (in the case of an aggressive patient), co-morbidities, infection control (think COVID!), communication with carers or parents of children, disagreement between clinical teams… the list is fairly extensive!
- To help you identify what this factor might be, when reading your clinical vignette, you should think about ‘what might be the spanner in the works here?’
Descriptor: ‘Was always flexible & open in manner when challenged’
- Always seek to understand what the other person is saying before reaching a conclusion
- Flexibility is the ability to alter your management plan as new information becomes available
Descriptor: ‘Was always aware of own limitations and where further help can be sought’
- It is important to remember that they only expect you to perform clinically at the level of an FY2 doctor. Even if you have taken years out of training after your foundation years and are capable of intubating a patient, you should call for help rather than proceeding with the intubation of a patient on your own.
- As with the point on team-working, think broadly about who you can call for help! Hospitals are full of allied health professionals with specialist skill sets to offer.
Descriptor: ‘Used effective strategies to deal with impact of others opinions/ questions’
- ICE (Ideas, Concerns, and Expectations) is generally used for communication with patients. However, if the scenario presents you with an anxious team member whose suggestions are not clinically appropriate, it may be worth exploring ICE with them. Perhaps they have had a bad experience in the past with similar patients and struggle to understand your rationale behind certain decisions.
- These strategies should never compromise patient safety
5. Commitment to Specialty
You should read around current topics in anaesthesia and understand the training pathway you are applying for.
Excellent knowledge of anaesthesia / ACCS training scheme, with a clearly defined career development plan to maximise training opportunities. Range of evidence to support intention to follow career in anaesthesia.
Descriptor: ‘Clear evidence of previous exposure to anaesthesia including undergraduate placements in anaesthesia / ICU, taster sessions, career open days’
- You should be able to give specific details about your exposure to anaesthesia, what drew you to want to pursue anaesthesia and what you learnt. Was there anything about the career that surprised you? Have you been taught to insert arterial or central lines?
- You should demonstrate multiple events of exposure to anaesthesia as a career (not just a one-off taster week)
- Did you receive any feedback from anaesthetic consultants while on your taster week?
Descriptor: ‘Good insight and knowledge regarding a career in anaesthesia and role of a core anaesthetic trainee’
- ‘Good insight’ means being able to talk about what you enjoy about anaesthesia and also some of the things that you may struggle with. Think of some pros and cons of the career – be realistic and honest – this will help you come across as balanced and mature in your decision to apply for anaesthetics training.
- Be sure to demonstrate an awareness that the role of the anaesthetist is far ranging beyond the walls of the theatre complex! Anaesthetists interact with almost every specialty in the hospital and have very particular technical and non-technical skill sets that are often called upon to deal with the sickest patients in the hospital.
Descriptor: ‘Clear evidence of knowledge of anaesthesia / ACCS training scheme applied’
- You should be aware that anaesthesia is an academically demanding specialty, and you will be credited as coming into the specialty with your eyes open if you mention the FRCA exams as a significant career goal or hurdle during your training years. If you have historically done well at medical school and won multiple prizes, you should not hold back in mentioning these achievements!
- You may be asked about whether you want to pursue dual-specialty training in intensive care medicine – there is no right or wrong answer, but if you do, you should be able to talk about how dual-specialty training works, when you would apply for a second training number and why you wish to dual-train intensive care with anaesthesia rather than another specialty.
Descriptor: ‘Demonstrated clear vision of opportunities available for career development within training program’
- Getting into anaesthetics training is only the first step. What else will you pursue once you have your Core/ ACCS Anaesthetics training number? Most activities make you a more well-rounded anaesthetist – but you must be clear about stating how and why you think so.
- Do you have any current interests that you would like to continue developing while in training (eg. teaching, instructing on ALS, audit, research, quality improvement, etc.) If you have past or ongoing achievements related to this, you should highlight it here.
- The RCoA and Association of Anaesthetists run various talks, courses and workshops throughout the year to complement training needs and enhance career development.
6. Involvement in Teaching, Audit, QI and Research
Audit, quality improvement and research are becoming a bigger focus in the new anaesthetic training curriculum. This has been reflected in the changes to the interview. Do not panic if you have not designed a whole project on your own and presented it at an international conference. The most important points are given for a showing that you understand what Audit/ QI/ Research are and why it is important. You should be able to discuss the differences between Audit/ QI/ Research and you should know the relevant steps for each of these.
Teaching is equally important as anaesthetists are often the educators that bring teams together. Even if you have not had major involvement in teaching programmes, you should be able to describe some form of educational activity that you have carried out either for medical students (eg. bedside teaching), physician associate students, nurses, healthcare assistants, or other allied health professionals. The scale of your teaching matters less than your
Descriptor: ‘Excellent description of major involvement in teaching activity undertaken and/ or teaching qualifications gained. Demonstrates clear ideas regarding role as an educator within anaesthetic training’
- The first part of this statement relates an outstanding answer with your ability to describe ‘major involvement’ in teaching. Do not simply state ‘I organised a national teaching course’. You should be able to describe it by explaining all the roles you played such as course registration, room-booking, organising the relevant speakers, planning the timetable for how the course would run, providing refreshments etc. All of these aspects of organising a course need to be spelt out to show the interviewers that you know what it involves and that you really did what you said you did.
- The second part of this statement talks about your role as an educator within anaesthetic training. As a specialty that interacts with almost every other specialty in the hospital, anaesthetists are best positioned to educate their multidisciplinary team members about common interests. In addition, as you become more senior in anaesthesia, you will find yourself teaching junior anaesthetists. The form of teaching in anaesthesia is unique in it’s largely one-to-one, hands-on style. It almost mirrors an apprenticeship or mentorship. This is why your engagement in teaching is important to the interviewers as all consultants teach on some level every day!
Descriptor: ‘Excellent description of audit / QI / research project undertaken with significant outputs (e.g. impact on change, presentations, publications)’
- You should be able to describe what your project was and why it was significant. Did you identify an issue within your department that affected you and so set out to fix it? What impact has your project had? Here, they have already listed you examples of how you can evidence that your project had ‘significant outputs’ – impact, presentations, publications.
- Do not fret if you did not lead a whole project on your own. Being a part of a team that achieved carrying out a project is just as valuable as long as you are able to describe all the roles you played in the team and demonstrate a clear understanding of the methodology of your project.
7. Qualifications and Experience
All qualifications and experience will count towards making you a better anaesthetist. Do not sell yourself short in this section of the interview.
As part of your preparation for your interview, make a list of any clinical experience you have had that is of particular interest (eg. Taster week, Anaesthetic job during foundation training, FY3 job or completion of part of training in another specialty) and list them in order of importance so that you mention your biggest achievements first.
In this same way, make and prioritise a list of non-clinical achievements – having climbed to the top of Everest will not necessarily earn you a higher score than if you conquered Snowdon. What is important is your ability to expound on the skills you learnt in the process and how they will make you a better doctor.
Medical training and clinical experience which is relevant to training in Anaesthesia
Descriptor: ‘Excellent description of qualifications required, plus additional qualifications relevant to anaesthesia (e.g. additional degrees / postgraduate qualifications). Comprehensive description of taster days & key placements as an undergraduate & postgraduate relevant to anaesthesia’
- An outstanding answer is one where you are able to do more than list your achievements. A ‘comprehensive description’ of any experience in anaesthesia will stand you apart from a typical answer. This means being able to tell your interviewer what you learnt, how it informed your decision to pursue this specialty, and what insights you gained about anaesthesia.
- Even if you feel that you have not done anything that you think is particularly ‘special’, you should be able to reflect on ANY experience to date and describe what you gained from it. The fact is that everyone entering this interview process has achieved something – part of your preparation for this interview is identifying formative points in your education and career to date.
- A well-thought out and reflective answer can include describing how obtaining your primary medical qualification itself is an achievement – the main point is this: do not undersell yourself!
8. Global Rating
This is an overall assessment of how candidates come across in their interview and how much evidence they provide for each claim they make about themselves. It often seems arbitrary, but there are concrete ways to work on this score. You will need to practice speaking out loud and be open to honest feedback from people you practice with.
This score relates to an assessor’s professional judgement of the overall performance of the applicant for the online interview. A score of 1 in this domain should be discussed between both assessors and the convener of the selection centre, to decide whether performance was so unsatisfactory that the applicant should be vetoed on this performance alone.
Descriptor: ‘Performance above standard in every respect e.g. exceptional ability for prioritising tasks, decision making, communication, team working and reflective practice, demonstrated by answers and examples given. Outstanding evidence of commitment to specialty’
- Practice speaking in a structured and collected manner.
- Be mindful of your non-verbal communication.
- Any claim you make about yourself should be evidenced – for example, ‘I am organised and punctual. In my MSFs throughout the last two years, people have often commented on my organisation and reliability as a colleague’. Simply saying ‘I am organised and punctual’ does not provide interviewers with the evidence they need to credit you the scores.
- Practice being reflective throughout your interview, as this domain is scored in both the clinical and general interview.
